Have you ever been hit on the inner part of the elbow and consequently felt severe electric pain referred down the inner side of the forearm down to the little finger?
That is neuropathic pain.
Neuropathic pain is defined by the International Society for the Study of Pain as:
Pain is caused by a disease or a lesion of the somatosensory system. That is, in the sensory nervous system.
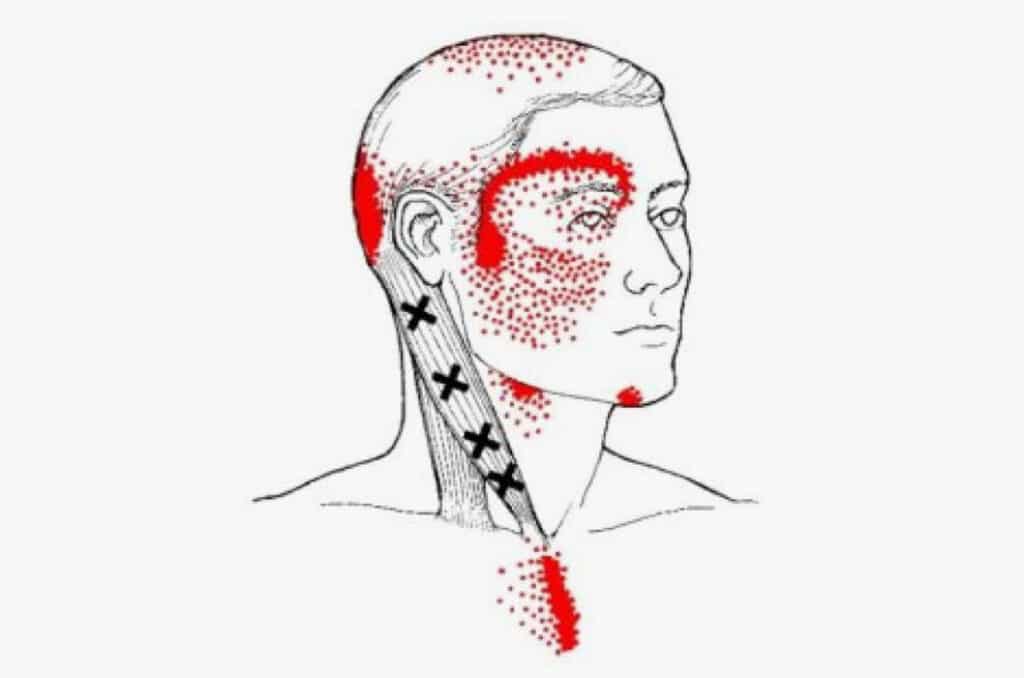
How does one know if pain is neuropathic or not? Neuropathic pain usually has certain characteristics. It is usually intolerable, is present all the time, has no relation to movement though may be exacerbated by even light touch, cold, wind or for no apparent reason at all. Because it is so severe, it is exhausting both physically and mentally. People with neuropathic pain tend to describe it as burning, freezing, hot, a sensation of needles, associated with itch or, ironically, numbness. There are descriptons of tingling or electrical sensations referred along the limb. In spite of this, there is no description that can absolutely ascertain that the pain is neuropathic and therefore in many cases it is difficult to diagnose the source of the pain. The pain can be localised or generalised. Localised pain can result from a peripheral nerve entrapment within scar tissue, an injury or from a viral infection such as Herpes zoster. Systemic diseases, such as diabetes, hepatitis C, chemotherapy treatment or certain vitamin deficiencies can cause the generalised type.
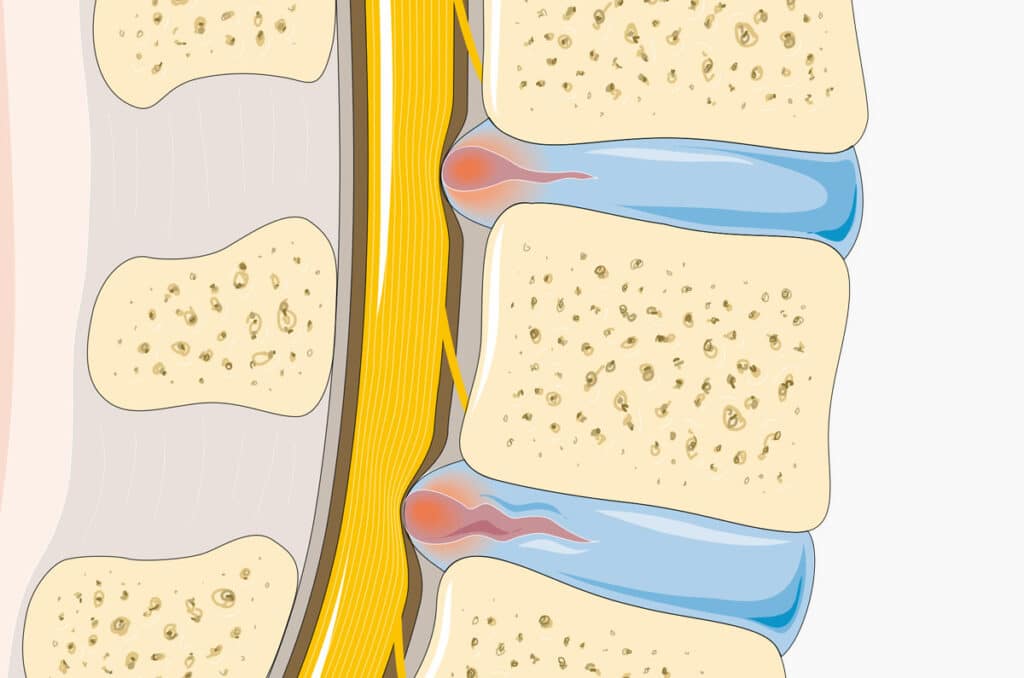
Because neuropathic pain is usually so chronic, the emotional reaction starts to exacerbate the pain. This is because the pain pathways tansmitting pain sensation to the brain join up with the pathways relaying emotion and pass through the thalamus, an area of the brain that interprets many of the negative experiences. Experience of pain and the experience of despair, frustration, anger and catastrophisation are all connected and affect one another.
Treatment of true neuropathic pain can be quite challenging. If there is a localised nerve entrapment by scar tissue, for example, one can perform a certain nerve block to release the entrapped nerve using a ‘hydrodissection’ technique, usually using a relatively large volume of injectate, depending on the region to be injected. This treatment is aimed at separating the entrapped nerve from the surrounding scar tissue, and can lead to long term improvement. Dr Wende tries exploit the body’s own healing mechanisms to bring about relief, thus reducing the need for several medications.
Treatment of neuropathic pain, especially the generalised type, must combine medications, rehabilitation, including occupational therapy, physiotherapy and psychological help in order to inhibit the facilitation of the pain to the brain. Because the emotional and mental aspect if the pain plays such a central role in pain sensation, treatment of negative emotional responses is important, even if the patient feels that he has no emotional problems. The interplay between both systems is physiological and one cannot deny it. Treatment may involve a combination of various medications which moderate the transmission of pain from the spinal cord to the brain. These medications do not necessarily eliminate the pain, but may reduce it , though many of these carry with them significant side effects.